Current best practices for environmental cleaning procedures in patient care areas, as well as cleaning for specific situations (e.g., blood spills) and for noncritical patient care equipment.
The materials on this page were created for use in global healthcare facilities with limited resources, particularly in low- and middle-income countries. U.S. healthcare facilities should reference other webpages for environmental cleaning resources.
This chapter provides the current best practices for environmental cleaning procedures in patient care areas, as well as cleaning for specific situations (e.g., blood spills) and for noncritical patient care equipment; see summary in Appendix B1 – Cleaning procedure summaries for general patient areas and Appendix B2 – Cleaning procedure summaries for specialized patient areas.
The determination of environmental cleaning procedures for individual patient care areas, including frequency, method, and process, should be based on the risk of pathogen transmission.
This risk is a function of the:
These three elements combine to determine low, moderate, and high risk—more frequent and rigorous (with a different method or process) environmental cleaning is required in areas with high risk. Risk determines cleaning frequency, method, and process in routine and contingency cleaning schedules for all patient care areas. This risk-based approach is outlined in Appendix A – Risk-assessment for determining environmental cleaning method and frequency.
Probability of contamination: Heavily contaminated surfaces and items require more frequent and thorough environmental cleaning than moderately contaminated surfaces, which in turn require more frequent and rigorous environmental cleaning than lightly or non-contaminated surfaces and items.
Vulnerability of patients to infection: Surfaces and items in care areas containing vulnerable patients (e.g., immunosuppressed) require more frequent and rigorous environmental cleaning than surfaces and items in areas with less vulnerable patients.
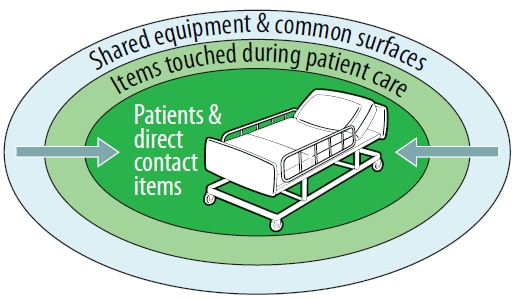
Potential for exposure to pathogens: High-touch surfaces (e.g., bed rails) require more frequent and rigorous environmental cleaning than low-touch surfaces (e.g., walls).
Every facility should develop cleaning schedules, including:
Checklists and other job aids are also required to ensure that cleaning is thorough and effective.
These aspects are covered in more detail in 2.4.3 Cleaning checklists, logs, and job aids.
For all environmental cleaning procedures, always use the following general strategies:
Proceed only after a visual preliminary site assessment to determine if:
Proceed from cleaner to dirtier areas to avoid spreading dirt and microorganisms. Examples include:
Proceed from high to low to prevent dirt and microorganisms from dripping or falling and contaminating already cleaned areas. Examples include:
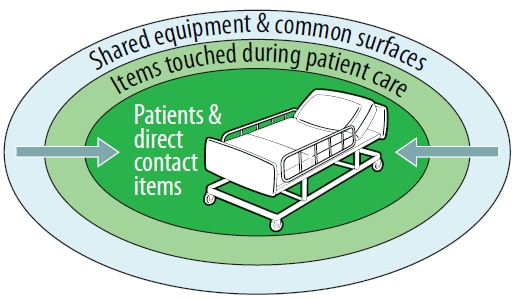
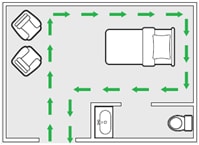
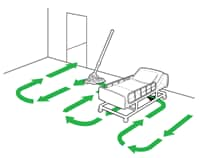
Proceed in a systematic manner to avoid missing areas—for example, left to right or clockwise (Figure 10).
In a multi-bed area, clean each patient zone in the same manner—for example, starting at the foot of the bed and moving clockwise.
Clean spills of blood or body fluids immediately, using the techniques in 4.5 Spills of blood or body fluids.
The identification of high-touch surfaces and items in each patient care area is a necessary prerequisite to the development of cleaning procedures, as these will often differ by room, ward and facility. See Appendix C – Example of high-touch surfaces in a specialized patient area. Perform assessments and observations of workflow in consultation with clinical staff in each patient care area to determine key high-touch surfaces.
Include identified high-touch surfaces and items in checklists and other job aids to facilitate completing cleaning procedures. See 2.4.3 Cleaning checklists, logs, and job aids.
General patient areas include:
Three types of cleaning are required for these areas:
Generally, the probability of contamination or the vulnerability of the patients to infection is low, so these areas may require less frequent and rigorous (e.g., method, process) cleaning than specialized patient areas.
General outpatient or ambulatory care wards include waiting areas, consultation areas, and minor procedural areas.
| Area | Frequency | Method | Process |
|---|---|---|---|
| Waiting / Admission | At least once daily (e.g., per 24-hour period) | Clean | High-touch surfaces and floors |
| Consultation / Examination | At least twice daily | Clean | High-touch surfaces and floors |
| Procedural (minor operative procedures; e.g., suturing wounds, draining abscesses) | Before and after (i.e., between [Footnote e]) each procedure |
Footnote e:
If there is prolonged time between procedures or local conditions that create risk for dust generation/dispersal, re-wipe surfaces with disinfectant solution immediately before the subsequent procedure.
Handwashing sinks, thoroughly clean (scrub) and disinfect
Sluice areas/sinks or scrub areas
Routine cleaning of inpatient areas occurs while the patient is admitted, focuses on the patient zones and aims to remove organic material and reduce microbial contamination to provide a visually clean environment.
Note: This occurs when the room is occupied, and systems should be established to ensure that cleaning staff have reasonable access to perform routine cleaning.
| Frequency | Method | Process |
|---|---|---|
| At least once daily (e.g., per 24-hour period) | Clean | High-touch surfaces and floors |
Terminal cleaning of inpatient areas, which occurs after the patient is discharged/transferred, includes the patient zone and the wider patient care area and aims to remove organic material and significantly reduce and eliminate microbial contamination to ensure that there is no transfer of microorganisms to the next patient.
Terminal cleaning requires collaboration between cleaning, IPC, and clinical staff to delineate responsibility for every surface and item, including ensuring that:
It is important that the staff responsible for these tasks are identified in checklists and SOPs to ensure that items are not overlooked because of confusion in responsibility.
| Frequency | Method | Process |
|---|---|---|
| Patient transfer or discharge | Clean and disinfect | See general terminal cleaning process below |
Scheduled cleaning occurs concurrently with routine or terminal cleaning and aims to reduce dust and soiling on low touch items or surfaces. Perform scheduled cleaning on items or surfaces that are not at risk for soiling under normal circumstances, using neutral detergent and water. But if they are visibly soiled with blood or body fluids, clean and disinfect these items as soon as possible.
| Frequency | Method | Process |
|---|---|---|
| Weekly | Clean | High surfaces (above shoulder height) such as tops of cupboards, vents |
Walls, baseboards and corners
Toilets in patient care areas can be private (within a private patient room) or shared (among patients and visitors). They have high patient exposure (i.e., high-touch surfaces) and are frequently contaminated. Therefore, they pose a higher risk of pathogen transmission than in general patient areas.
Toileting practices vary, in terms of both the types of toilets in use (e.g., squat or sit, wet or dry) and the adherence to correct use. Therefore, needs for cleaning and disinfection vary. In some cases, more than twice daily cleaning and disinfection may be warranted.
Depending on resource and staffing levels, dedicated cleaning staff posted at shared toilets in healthcare facilities could reduce risk associated with these areas.
| Area | Frequency | Method | Process |
|---|---|---|---|
| Private toilets | At least once daily (e.g., per 24-hour period), after routine cleaning of patient care area | Clean and disinfect | High-touch and frequently contaminated surfaces in toilet areas (e.g., handwashing sinks, faucets, handles, toilet seat, door handles) and floors |
| Public or shared toilets (e.g., patients, visitors, family members) | At least twice daily | Clean and disinfect | High-touch and frequently contaminated surfaces in toilet areas (e.g., handwashing sinks, faucets, handles, toilet seat, door handles) and floors |
| Both (private and shared) | Scheduled basis (e.g., weekly) and when visibly soiled | Clean | Low-touch surfaces; see 4.2.4 Scheduled cleaning |
Floors generally have low patient exposure (i.e., are low-touch surfaces) and pose a low risk for pathogen transmission. Therefore, under normal circumstances they should be cleaned daily, but the use of a disinfectant is not necessary.
There are situations where there is higher risk associated with floors (e.g., high probability of contamination), so review the specific procedures in 4.2 General patient areas and 4.6 Specialized patient areas for guidance on frequency of environmental cleaning of floors and when they should also be disinfected.
| Area | Frequency | Method | Process |
|---|---|---|---|
| Floors in general inpatient and outpatient areas, always cleaned last after other environmental surfaces | At least once daily (e.g., per 24-hour period) or as often as specified in the specific patient care area | Clean (unless otherwise specified within specific patient care area) | See general mopping process below |
Regardless of the risk-level of an area, spills or contamination from blood or body fluid (e.g., vomitus), must be cleaned and disinfected immediately using a two-step process.
Specialized patient areas include those wards or units that provide service to:
This vulnerable population is more prone to infection and the probability of contamination is high, making these areas higher risk than general patient areas.
Unless otherwise indicated, environmental surfaces and floors in the following sections require cleaning and disinfection with a facility-approved disinfectant for all cleaning procedures described.
Operating rooms are highly specialized areas with a mechanically controlled atmosphere where surgical procedures are performed. These require environmental cleaning at three distinct intervals throughout the day:
Because operating rooms are highly specialized areas, the surgery department clinical staff usually manages environmental cleaning. Operating room nurses and their assistants sometimes perform cleaning duties along with, or sometimes instead of, general cleaning staff.
Critical and semi-critical equipment in the operating rooms require specialized reprocessing procedures and are never the responsibility of environmental cleaning staff. The processes described below pertain only to the cleaning and disinfection of environmental surfaces and the surfaces of noncritical equipment.
Where multiple staff are involved, clearly defined and delineated cleaning responsibilities must be in place for cleaning of all environmental surfaces and noncritical patient care equipment (stationary and portable). The use of checklists and SOPs is highly recommended.
| Frequency | Process |
|---|---|
| Before the first procedure | Carefully inspect records and assess the operating space to ensure that the terminal clean was completed the previous evening. |
Wipe all horizontal surfaces in the room (e.g., furniture, surgical lights, operating bed, stationary equipment) with a disinfectant to remove any dust accumulated overnight.
If there was no written confirmation or terminal cleaning on the previous day, do a full terminal clean (see Terminal Clean on this table).
Thoroughly clean and disinfect portable patient-care equipment that is not stored within the operating room, such as suction regulators, anesthesia trolley, compressed gas tanks, x-ray machines, and lead gowns, before introduction into the operating room.
Clean and disinfect:
Thoroughly clean and disinfect portable patient-care equipment that is not stored within the operating room before removal from the operating room. Examples include:
Have dedicated supplies and equipment for the OR (e.g., mops, buckets).
Use fresh mops/floor cloths and mopping solutions for every cleaning session, including between procedures.
Use fresh cleaning cloths for every cleaning session, regularly replacing them during cleaning and never double-dipping them into cleaning and disinfectant solutions.
Departments or areas where medication is prepared (e.g., pharmacy or in clinical areas) often service vulnerable patients in high-risk and critical care areas, in addition to other patient populations.
The staff who work in the medication preparation area might be responsible for cleaning and disinfecting it, instead of the environmental cleaning staff.
Develop detailed SOPs and checklists for each facility to identify roles and responsibilities for environmental cleaning in these areas.
| Frequency | Process |
|---|---|
| Before and after every use | Countertops and portable carts used to prepare or transport medications |
| At least once every 24 hours | All high-touch surfaces (e.g., light switches, countertops, handwashing sinks, cupboard doors) and floors |
| Scheduled basis (e.g., weekly, monthly) | Low-touch surfaces, such as the tops of shelves, walls, vents |
Departments or areas where semi-critical and critical equipment is sterilized and stored (i.e., sterile services) often service vulnerable patients in high-risk and critical care areas, in addition to other patient populations.
Staff who work in the SSD might be responsible for cleaning and disinfecting it instead of environmental cleaning staff. Alternatively, it is possible to train and assign a dedicated cleaning staff member to this area.
Develop detailed SOPs and checklists for each facility to identify roles and responsibilities for environmental cleaning in these areas.
| Frequency | Process |
|---|---|
| Before and after every use | Utility sinks used for washing medical devices (e.g., endoscopes) |
| At least twice daily | All high-touch surfaces (e.g., countertops, surfaces of washing equipment, handwashing sinks) and floors |
| Scheduled (e.g., weekly, monthly) | Low-touch surfaces, such as the tops of shelves, walls, vents |
SSDs have two distinct areas, the soiled area (also called dirty area or decontamination area) and the clean area.
Intensive care units (ICUs) are high-risk areas due to the severity of disease and vulnerability of the patients to develop infections.
Frequency and process is the same for adult, pediatric, and neonatal units, but there are specific considerations for neonatal areas. See Process / Additional guidance in Table 16 below.
| Frequency | Process / Additional guidance |
|---|---|
| Twice daily and as needed | Clean and disinfect high-touch surfaces |
Clean floors with neutral detergent and water
If a neonatal incubator is occupied, clean and disinfect only the outside; only clean (neutral detergent) on inside
Ensure that cleaning schedules details responsible staff (e.g., nursing or cleaning staff) for environmental cleaning of surfaces of noncritical patient care equipment
Last clean of the day: also clean low-touch surfaces; see 4.2.4 Scheduled cleaning
Change filters in incubators according to manufacturer’s instructions, when wet or if neonate was on contact precautions (during terminal clean)
Pay special attention to terminal cleaning of incubators
Pay special attention to ensure reprocessing of noncritical patient care equipment
Provide dedicated supplies and equipment for the ICU (e.g., mops, buckets) that are not used anywhere else.
Use fresh mops/floor cloths and mopping solutions for every cleaning session.
Use fresh cleaning cloths for surfaces for every cleaning session (at least two per day), regularly replacing them during cleaning and never double-dipping into cleaning and disinfectant solutions.
Emergency departments are moderate to high-risk areas because of the wide variability in the condition of patients and admissions, which can:
Because emergency departments are specialized and high-throughput areas, clinical staff (e.g., nurses) might play an active role in performing environmental cleaning, particularly in examination and procedural areas.
Develop detailed SOPs, including checklists for each facility to identify roles and responsibilities for environmental cleaning in these areas.
| Area | Frequency | Process |
|---|---|---|
| Waiting / Admission | At least once daily (e.g., per 24-hour period) | High-touch and low-touch surfaces and floors |
| Consultation / Examination (low acuity) | After each event/case and at least twice daily, and as needed | High-touch surfaces |
End of the day: entire floor and low-touch surfaces
Before and after (i.e., between*) each procedure*If there is prolonged time between procedures or local conditions that create risk for dust generation/dispersal, re-wipe surfaces with disinfectant solution immediately before the subsequent procedure.
All surfaces and the entire floorHandwashing sinks (thoroughly clean (scrub) and disinfect)
Sluice areas/sinks or scrub areas
Labor and delivery wards are routinely contaminated and patients are vulnerable to infection.
Because labor and delivery wards are often high-throughput areas, clinical staff (e.g., nurses) might play an active role in performing environmental cleaning, particularly between procedures.
Develop detailed SOPs, including checklists, for each facility to identify roles and responsibilities for environmental cleaning in these areas.
Remove soiled linens and waste containers for disposal/reprocessing; see Appendix D – Linen and laundry management
Clean and disinfect:
Clean and disinfect other high-touch surfaces (e.g., light switches, door handles) outside of the patient zone
Clean (scrub) and disinfect handwashing sinks
Clean and disinfect entire floor (move patient bed and other portable equipment)
The areas in this section are higher risk because of:
Nursing and cleaning staff might be responsible for cleaning certain areas/items in these areas, so there must be clearly defined cleaning responsibilities for all surfaces and equipment (stationary and portable).
Develop detailed SOPs, including checklists, for each facility to identify roles and responsibilities for environmental cleaning in these areas.
Remove disposable patient care items/waste and reprocess reusable noncritical patient care equipment; see Table 26. Recommended Selection and Care of Noncritical Patient Care Equipment
Clean and disinfect:
Remove soiled linens and waste containers for disposal/reprocessing; see Appendix D – Linen and laundry management
Clean and disinfect:
Last clean of the day: clean and disinfect entire floor and low-touch surfaces
Clean floors with neutral detergent and water
Remove disposable equipment and reprocess reusable noncritical patient care equipment; see Table 26. Recommended Selection and Care of Noncritical Patient Care Equipment.
Clean and disinfect:
Clean and disinfect:
Isolation or cohorted areas with suspected or confirmed cases of infections requiring transmission-based precautions are considered high-risk areas, particularly for:
The three types of transmission-based precautions are:
Transmission-specific PPE is required for all cleaning sessions in areas under transmission-based precautions, according to facility policy or Table 5 in 3.4 Cleaning Supplies and Equipment.
PPE should always be put on and removed following the indications posted/recommended by IPC.
A full list of pathogens/infections requiring these precautions are included in CDC's Guideline for Isolation Precautions.
Unit manager or shift leader should coordinate schedule
Take care to keep the door closed during the cleaning process (ventilation requirement)
Unit manager or shift leader should coordinate schedule
Take care to keep the door closed during the cleaning process (ventilation requirement)
Any surface (e.g., walls) that is visibly soiled with blood or body fluids
See Cleaning for C. difficile (spore forming)
Last clean of the day: clean and disinfect low-touch surfaces
These organisms belong to a group of carbapenem-resistant, gram-negative bacteria of national and international concern because of their implication as an emerging cause of severe healthcare-associated infections. In 2017, the World Health Organization published the first global guidelines for the prevention and control of CRE-CRAB-CRPsA in healthcare facilities, which include environmental cleaning and disinfection as a key recommendation.
This implementation guide discusses the key elements of environmental cleaning needed for prevention and control of these organisms: WHO 2019: Implementation manual to prevent and control the spread of carbapenem-resistant organisms at the national and health care facility level [PDF – 98 pages] .
There might be specific cleaning procedures for isolation areas of highly infectious pathogens. Standalone training programs and strict adherence to required PPE is essential for conducting effective environmental cleaning in these situations.
Find more information on developing context-specific protocols:
Portable or stationary noncritical patient care equipment incudes IV poles, commode chairs, blood pressure cuffs, and stethoscopes. These high-touch items are:
Critical and semi-critical equipment requires specialized reprocessing procedures and is never the responsibility of environmental cleaning staff.
 include stethoscopes and bedpans." />
include stethoscopes and bedpans." />
The responsibility for cleaning noncritical patient care equipment might be divided between cleaning and clinical staff, so it is best practice to clearly define and delineate cleaning responsibilities for all equipment (stationary and portable).
Develop a cleaning chart or schedule outlining the method, frequency, and staff responsible for cleaning every piece of equipment in patient care areas and take care to ensure that both cleaning and clinical staff (e.g., nursing) are informed of these procedures so that items are not missed.
| Type of Equipment | Frequency | Method | Additional Guidance |
|---|---|---|---|
| Shared (e.g., general inpatient wards) | Before and after each use | Clean and disinfect | Select a compatible disinfectant; see 4.7.1 Material compatibility considerations |
Clean and disinfect heavily soiled items (e.g., bedpans) outside of the patient care area in dedicated 4.7.2 Sluice rooms
Disinfect bedpans with a washer-disinfector or boiling water instead of a chemical disinfection process.
Clean and disinfect heavily soiled items (e.g., bedpans) outside of the patient care area in dedicated 4.7.2 Sluice rooms
Disinfect bedpans with a washer-disinfector or boiling water instead of a chemical disinfection process
A list of compatible cleaning and disinfectant products should be included in manufacturer's instructions or provided by the manufacturer upon request.
If manufacturer instructions are not available, here are the applicable material compatibility considerations and best practices for use of common healthcare disinfectants:
Each major patient care area should be equipped with a designated sluice room to reprocess soiled noncritical patient care equipment (e.g., commode chairs, bedpans). Alternatively, there may be central depots where these procedures are performed.
Sluice rooms should be as close as possible to the patient care areas that they serve and should have an organized workflow from soiled (dirty) to clean.
| Type of Equipment | Frequency | Method | Additional Guidance |
|---|---|---|---|
| Soiled areas | At least once daily (e.g., per 24-hours period) | Clean and disinfect | High-touch and frequently contaminated surfaces, including work counters and sinks, and floors (floors only require cleaning) |
| Clean area | At least once daily (e.g., per 24-hours period) | Clean | Horizontal surfaces and floors |
Clean equipment should be covered or removed during cleaning process
It is best practice to perform routine, standardized assessments of environmental cleaning (i.e., practices, level of cleanliness) in order to:
This section includes an overview of the available methods, as well as their advantages and disadvantages. The best practices for developing a system of routine monitoring, audit, and feedback within environmental cleaning program implementation are covered in 2.5 Monitoring, feedback, and audit elements.
| Method | Advantages | Disadvantages |
|---|---|---|
| Performance observations: observers (e.g., cleaning supervisors) use standardized perform structured observations using checklists that are specific to individual patient care areas. The goal is to rate the effectiveness of cleaning staff and adherence to the SOP (such as identifying the number of steps performed correctly). | Can be used for large areas (units, wards) |
Easy to implement
Benchmarking is possible
Simple and inexpensive
Allows immediate and direct feedback to individual staff
Encourages cleaning staff engagement and input
Identifies gaps for staff training/job aid improvements
Subjective—difficulty in standardizing methodology and assessment across observersResults affected by Hawthorne bias (i.e., more of an assessment of knowledge than actual practice)
Does not assess or correlate to bioburden
Easy to implement
Benchmarking is possible
Allows immediate and direct feedback to individual staff
Could be delay in feedback dependent on method used to compile resultsSubjective—based on individual determinations of dust/debris levels
Does not assess or correlate to bioburden
Provides immediate feedback on performance
Minimal training required to perform
Benchmarking is possible
Does not assess or correlate to bioburdenLabor-intensive as surfaces should be marked before cleaning and checked after cleaning has been completed
Some difficulties documented in terms of removal of markers from porous or rough surfaces (e.g., canvas straps)
Need to vary frequency and objects to prevent monitoring system from becoming known
Provides immediate feedback
Minimal training required to perform
Low sensitivity and specificity
Lacks a standardized threshold or benchmark for determining the level or status of cleanliness (i.e., “safe” post-cleaning ATL levels) for specific surfaces or patient care areas
Technology constantly changing
Interference of cleaning products, supplies and in some cases surfaces, which can both reduce or enhanced ATP levels (e.g., bleach, microfiber, stainless steel)
High sensitivity and specificityProvides direct indication of presence of specific pathogens (direct swab cultures)
May be useful for identifying source of outbreaks and/or environmental reservoirs
Not recommended for routine useProlonged time for results (>48hrs)
Requires access to laboratory resources and trained personnel for interpreting results
Lack of defined threshold or benchmark for determining the level or status of cleanliness (e.g., colony-forming units per surface area)